The Real Reason Biden Extended the “National Emergency” for COVID
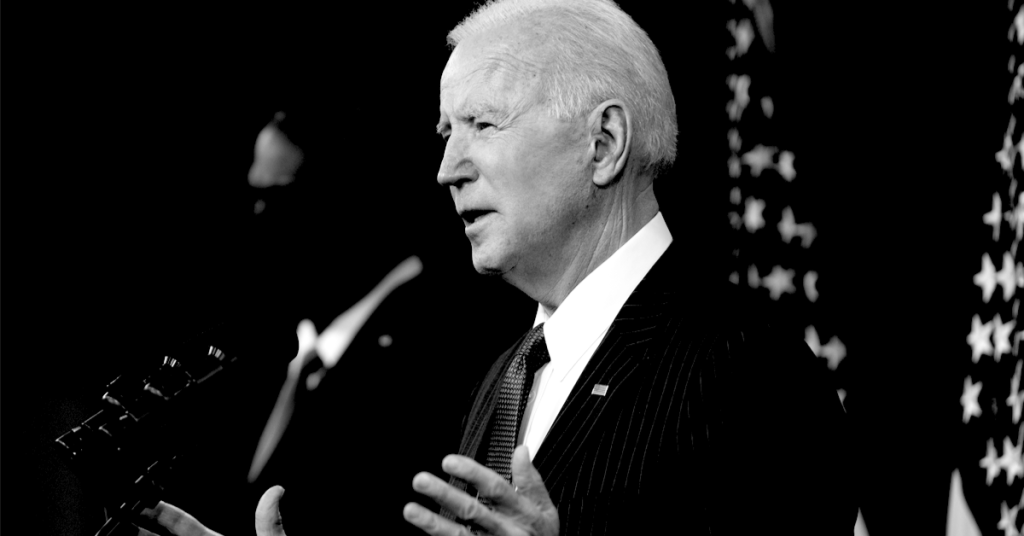
As countries around the world are dropping COVID restrictions and downgrading the virus to “flu-like status,” President Joe Biden announced on Feb. 18 the U.S. national emergency declared in March 2020 for COVID will be extended beyond March 1.
Citing the ongoing risk to “public health and safety” posed by the virus, Biden told House Speaker Nancy Pelosi (D-CA) — in a letter released by the White House — there “remains a need to continue this national emergency.”
“The COVID-19 pandemic continues to cause significant risk to the public health and safety of the Nation. More than 900,000 people in this Nation have perished from the disease, and it is essential to continue to combat and respond to COVID-19 with the full capacity and capability of the Federal Government,” he wrote. “Therefore, in accordance with section 202(d) of the National Emergencies Act (50 U.S.C. 1622(d)), I am continuing the national emergency declared in Proclamation 9994 concerning the COVID-19 pandemic.”
“For this reason, the national emergency declared on March 13, 2020, and beginning March 1, 2020, must continue in effect beyond March 1, 2022,” Biden wrote in a second statement released by the White House for publication in the Federal Register.
The emergency would have been automatically terminated unless, within 90 days prior to the anniversary date of its declaration, Biden notified Congress of his intent that it continue beyond the anniversary date.
What’s really behind the national emergency extension for COVID
Continuing to classify COVID as an indefinite “national emergency” allows pharmaceutical companies to cut corners, escape liability and rake in billions. It’s really that simple.
The real reason Biden continued COVID’s “national emergency status” is because numerous COVID vaccines and drugs are authorized by the U.S. Food and Drug Administration (FDA) under Emergency Use Authorization (EUA).
According to the FDA’s website, EUA authority “allows FDA to help strengthen the nation’s public health protections against chemical, biological, radiological and nuclear threats including infectious diseases, by facilitating the availability and use of medical countermeasures needed during public health emergencies.”
For a product to receive EUA, there must be a public health emergency, and if the “circumstances that precipitated the declaration” cease, products approved under EUA lose their authorization.
Currently, the only COVID vaccines available in the U.S. are authorized for emergency use. In addition, Merck’s COVID pill “Molnupiravir,” Pfizer and Gilead’s Remdesivir and Pfizer’s Paxlovid are all under EUA.
A multi-billion dollar industry is reliant on the indefinite continuation of a national emergency or their products can’t be used.
In addition, it is essential to continue emergency status to protect COVID vaccine manufacturers from liability. While under Emergency Use Authorization, COVID vaccines are subject to the Public Readiness and Emergency Preparedness Act, which indemnifies vaccine makers for the harms caused by their products and prohibits the vaccine-injured from recovering meaningful damages.
Biden’s decision to extend the emergency comes as Omicron cases drop and countries around the world announce they are lifting COVID restrictions — downgrading COVID to “endemic status” and returning to their pre-pandemic lives.
Several Democratic governors recently announced they were rescinding COVID mandates, including vaccine passports and mask requirements. New York, Massachusetts, New Jersey, California, Connecticut, Delaware and Oregon have all taken similar actions.
A recent Monmouth University poll showed 70% of Americans believe, “It’s time we accept that COVID is here to stay and we just need to get on with our lives.”
It is unknown what would need to occur for the Biden administration to end the national emergency, but it’s reasonable to expect the “emergency” will not end as long as billion-dollar pharmaceutical companies who fund U.S. health agencies rely on Emergency Use Authorization for their products.